Dr. Debasis Maity
Consultant Uro-Surgeon
Medical Discussion
Renal Stone
- Stone occurrence is uncommon before age 20, but peaks in incidence in the fourth to sixth decades of life.
- Male-to-female ratio of 1.8 among Asians.
- Higher prevalence of stone disease is found in hot, arid, or dry climates such as the mountains, desert, or tropical areas.
- Areas of high stone prevalence included the United States, British Isles, Scandinavian and Mediterranean countries,
northern Indiaand Pakistan, northern Australia, Central Europe, portions of the Malay peninsula and China. - Patient with higher BMI excreted
more urinary oxalate, uric acid, sodium and phosphorusthan those with lower BMI. - The association of obesity and uric acid stone formation is primarily influenced by urinary pH.
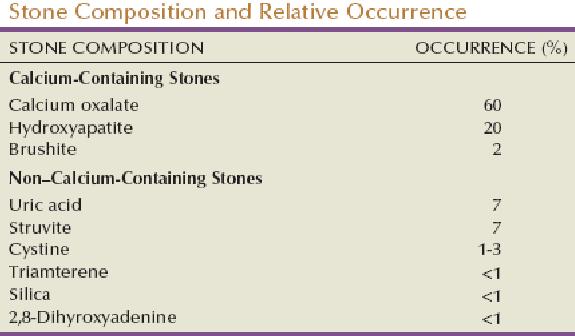
Classification of Nephrolithiasis:
The most common component of urinary calculi is calcium, which is a major constituent of nearly 75% of stones. Calcium oxalate makes up about 60% of all stones; mixed calcium oxalate and hydroxyapatite, 20%; and brushite stones, 2%.
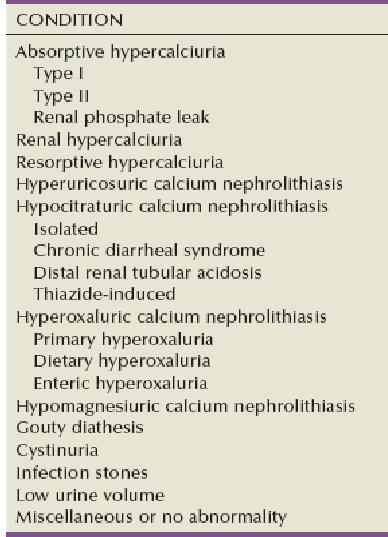
Diagnostic classification:
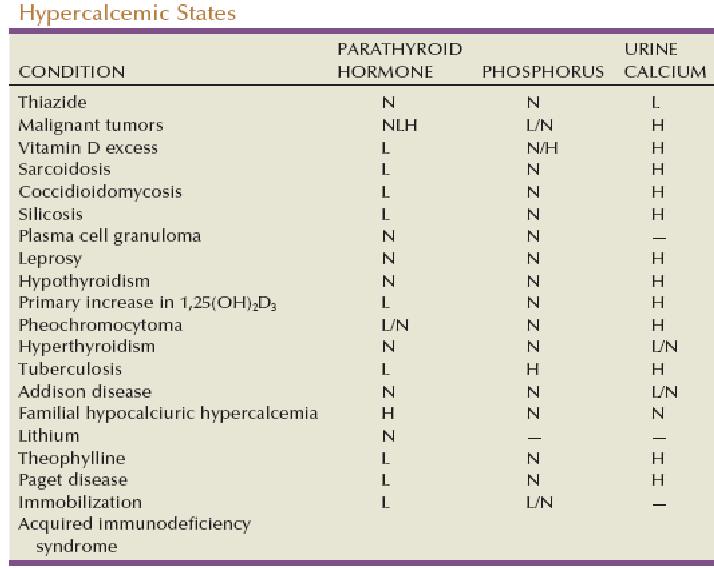
Conditions associated with hypercalcemia:
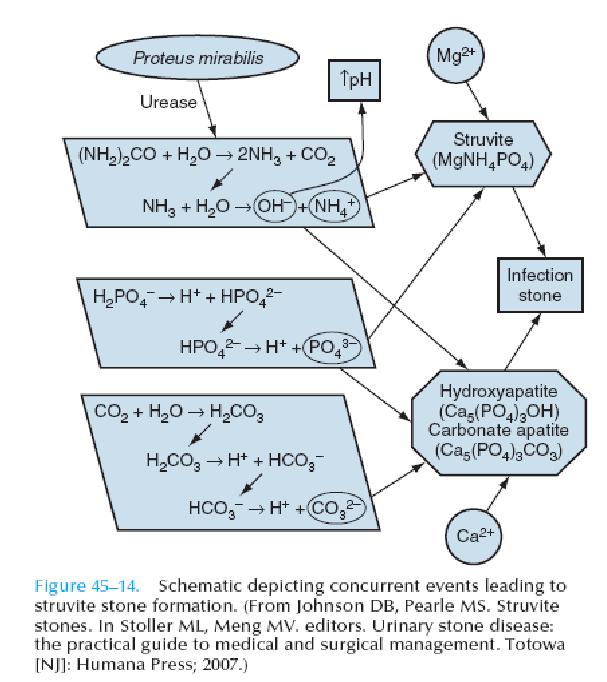
Struvite stone formation:
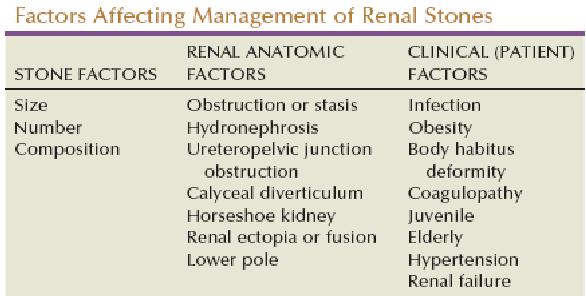
Anatomic predisposition for stone:
- PUJO
- Horseshoe kidney
- Calyceal diverticula
- Stone in pregnancy
Diagnostic evaluation:
- Indications for a Metabolic Stone Evaluation:
- Recurrent stone formers
- Strong family history of stones
- Intestinal disease (particularly chronic diarrhea)
- Pathologic skeletal fractures
- Osteoporosis
- History of urinary tract infection with calculi
- Personal history of gout
- Infirm health (unable to tolerate repeat stone episodes)
- Solitary kidney
- Anatomic abnormalities
- Renal insufficiency
- Stones composed of cystine, uric acid, struvite
- Evaluation of Single Stone Formers
- History
- Underlying predisposing conditions
- Medications (calcium, vitamin C, vitamin D, acetazolamide, steroids)
- Dietary excesses, inadequate fluid intake or excessive fluid loss
- Multichannel blood screen:
- Basic metabolic panel = (sodium, potassium, chloride, carbon dioxide, blood urea nitrogen, creatinine)
- Calcium
- Intact parathyroid hormone
- Uric acid
- Urinalysis:
- pH > 7.5: infection lithiasis
- pH < 5.5: uric acid lithiasis
- Sediment for crystalluria
- Urine culture
- Urea-splitting organisms: suggestive of infection lithiasis.
- Qualitative cystine
- Radiography: (X-ray, NCCT, IVP)
- Radiopaque stones: calcium oxalate, calcium phosphate, magnesium ammonium phosphate (struvite), cystine
- Radiolucent stones: uric acid, xanthine, triamterene
- Intravenous pyelography: radiolucent stones, anatomic abnormalities
- Stone analysis
Microscopic Appearance of Common Urinary Calculi:
| Chemical Type | Appearance |
|---|---|
| Calcium oxalate monohydrate | Hourglass |
| Calcium oxalate dihydrate | Envelope, tetrahedral |
| Calcium phosphate-apatite | Amorphous |
| Brusite | Needle shaped |
| Magnesium ammonium phosphate (struvite) | Rectangular, coffin-lid |
| Cystine | Hexagonal |
| Uric acid | Amorphous shards, plates |
Differential Diagnosis of Hypercalciuria:
| Points | Absorptive | Renal | Resorptive |
|---|---|---|---|
| Serum calcium | Normal | Normal | Elevated |
| Parathyroid Function | Suppressed | Stimulated | Stimulated |
| Fasting urinary calcium | Normal | ↑ | ↑ |
| Intestinal Calcium absorption | ↑ | ↑ | ↑ |
Hypercalciuria (>200 mg/day):
The classification of nephrolithiasis recognizes three broad categories of hypercalciuria.
Absorptive Hypercalciuria:Absorptive Hypercalciuria involves an increase in the amount of calcium that is absorbed by the intestinal tract.Renal Hypercalciuria:Renal hypercalciuria (RH) (also known as renal leak hypercalciuria) is thought to be due to a wasting of calcium by the functioning nephron.Resorptive Hypercalciuria(Primary Hyperparathyroidism): Patients with this disorder suffer from an overproduction of parathyroid hormone from either one dominant adenoma or from diffuse hyperplasia of all four glands.
Hyperuricosuric Calcium Nephrolithiasis:
Patients with hyperuricosuria may be prone to the formation of calcium oxalate calculi through a process called heterogeneous nucleation (also referred to as epitaxy).
Hyperoxaluria (>40 mg/day):
Enteric Hyperoxaluria- This entity is often one of the most striking findings during a metabolic evaluation because it involves multiple factors, all caused as a result of chronic diarrhea with its attendant dehydration and bicarbonate losses.
Hypocitraturic Calcium Nephrolithiasis:
- <550 mg in female
- <450 mg in male
Causes of Acquired Renal Tubular Acidosis:
- Obstructive uropathy
- Recurrent pyelonephritis
- Acute tubular necrosis
- Renal transplantation
- Analgesic nephropathy
- Sarcoidosis
- Idiopathic hypercalciuria
- Primary hyperparathyroidism.
High Oxalate Foods are-
- Tea (black)
- Cocoa
- Spinach
- Mustard greens
- Pokeweed
- Swiss chard
- Beets
- Rhubarb
- Okra
- Berries (some)
- Chocolate
- Nuts
- Wheat germ
- Soy crackers
- Pepper
Hypomagnesiuric Calcium Nephrolithiasis (<80 mg):
Hypomagnesiuric calcium nephrolithiasis is characterized by low urinary magnesium, hypocitraturia, and low urine volume.
Cystinuria:
Cystinuria is caused by an autosomal recessive error of transepithelial transport involving the intestine and the kidneys.
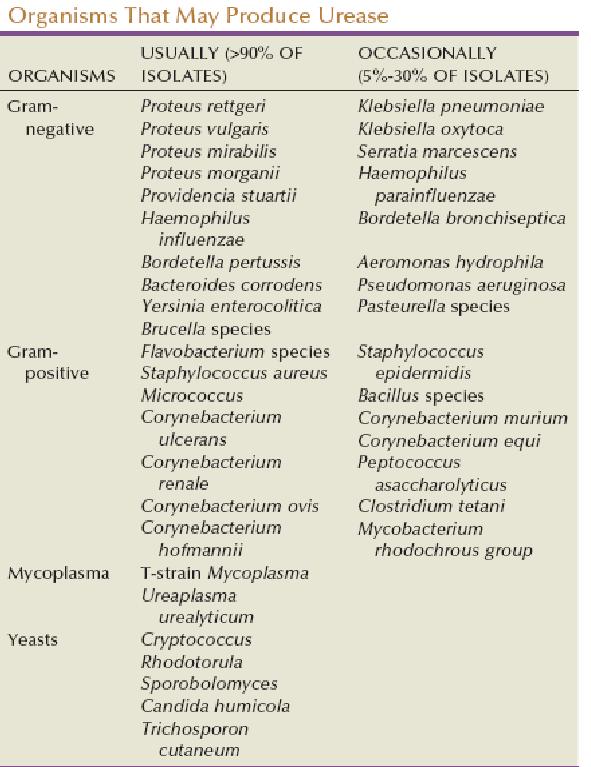
Infection Calculi (Struvite):
Struvite calculi form in the presence of alkaline urine (pH above 7.2) and in an environment rich in ammonia. The ammonia is thought to be produced via the splitting of urea by colonization with bacteria that produce urease.
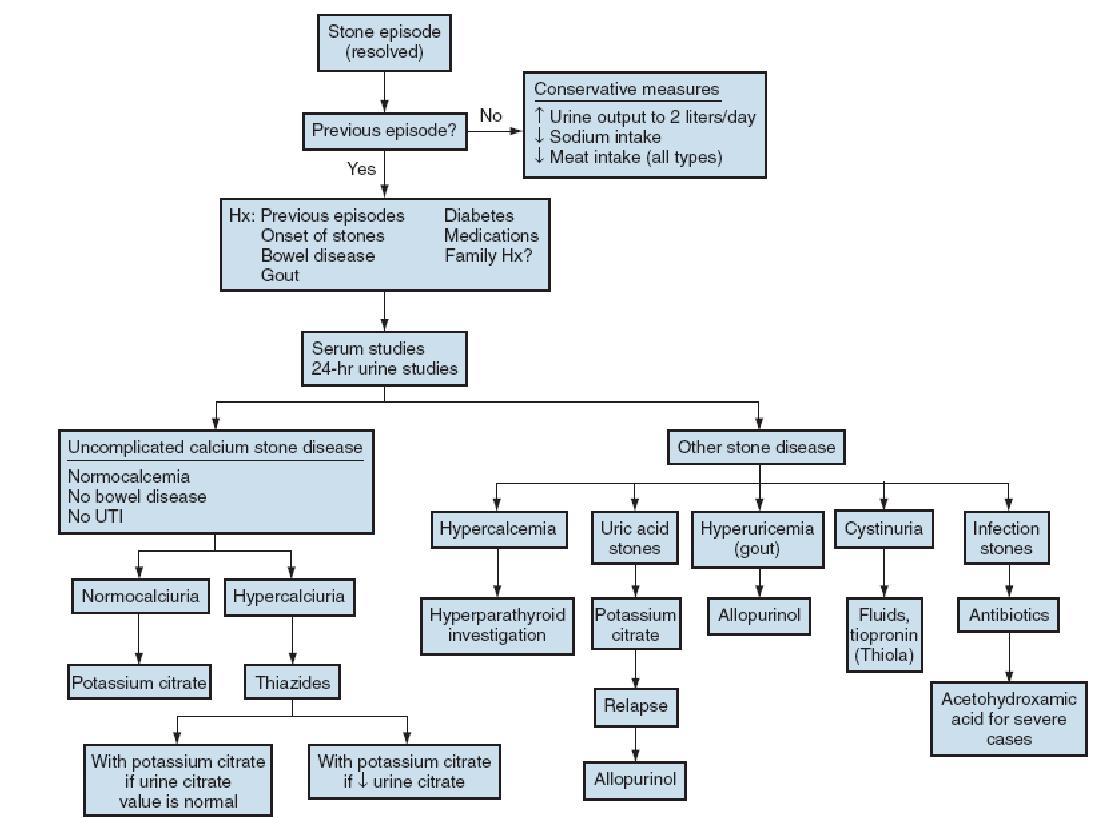
Medical management of stones:
- One mainstay of conservative management is the forced increase in fluid intake to achieve a daily urine output of 2 L. (
to drink 3 litres/day). - Carbonated water may confer some protective benefit.
- Soda flavored with phosphoric acid may increase stone risk, whereas those with citric acid may decrease risk.
Citrus juices(particularlylemonand orange juices) may be a useful adjunct to stone prevention.- Reduced animal protein (meat) intake.
- A diet high in fruits and vegetables imparts a reduced risk of stone formation.
- Dietary sodium restriction in both normal volunteers and stone formers.
- Obesity is an independent risk factor for nephrolithiasis, particularly for women.
- Metabolic syndrome is associated with lower urinary pH.
- Obese patients have a higher propensity for uric acid calculi.
- High-protein, low-carbohydrate diets alter urinary parameters and may increase the risk of stone formation.
- Even modern bariatric surgery may significantly increase the overall risk of stone formation.
- Dietary calcium restriction actually increases stone recurrence risk.
Calcium supplementation is likely safest when taken with meals.Calcium citrate appears to be a more “stone-friendly” calcium supplement due to the additional inhibitor action of citrate.- Avoidance of excess dietary oxalate loading is reasonable and intuitive.
- Vitamin C in large doses may increase the risk of stone recurrence. Doses should probably be limited to 2 g/day.
- Bladder calculi are best managed with endoscopic techniques.
- Subsequent recurrence is prevented by relief of the bladder outlet obstruction.
- Neonatal nephrocalcinosis is frequently caused by loop diuretics. Cessation of this medication is essential.
- Neonatal nephrocalcinosis may be reversed by the use of thiazides.
- The majority of ureteral calculi during pregnancy pass spontaneously.
- There is a growing trend toward endoscopic relief of symptomatic calculi during pregnancy.
Surgical management of Stones:
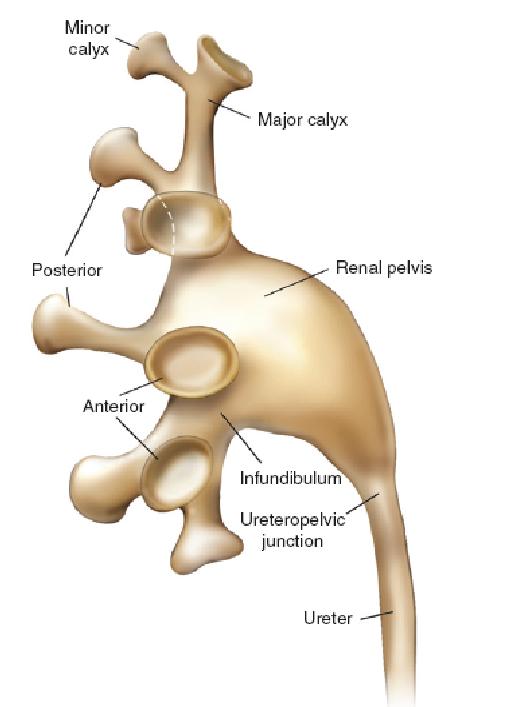
Renal Calyceal Anatomy:
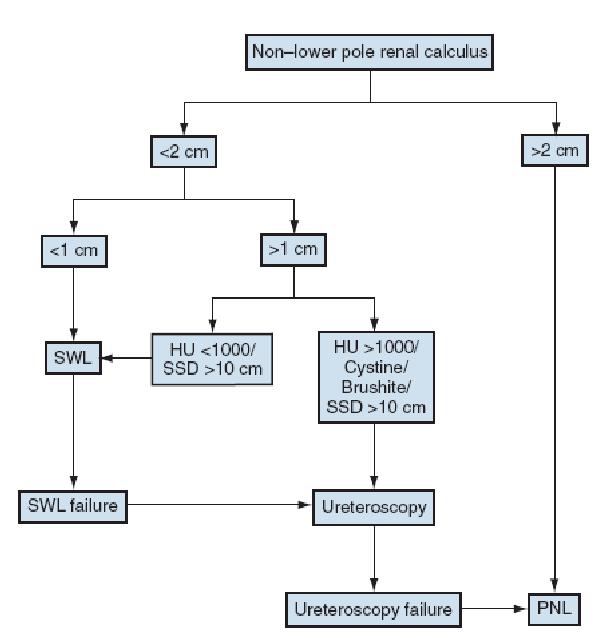
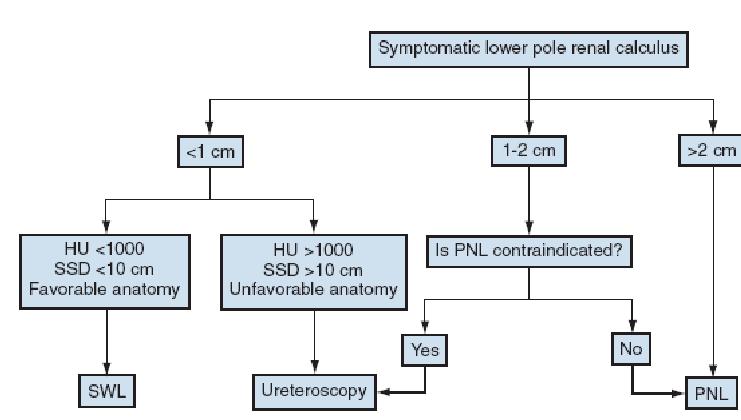
Algorithm for management of Renal Stone:
1.
2.
Renal Side Effects of Shockwave Lithotripsy:
Acute Histologic Changes-- Venous thrombi
- Cellular disruption and necrosis
- Mild tubular necrosis (ischemic changes)
- Intraparenchymal hemorrhage
- Tubular dilation and cast formation
- Damage and rupture of veins and small arteries
- Rupture of glomerular and peritubular capillaries.
Chronic Histologic Changes-- Nephron loss
- Dilated veins
- Streaky fibrosis
- Diffuse interstitial fibrosis
- Calcium and hemosiderin deposits
- Hyalinized and acellular scars from cortex to medulla
Acute Renal Side Effects: Risk Factors for Shockwave Lithotripsy:
- Age
- Obesity
- Coagulopathies
- Thrombocytopenia
- Diabetes mellitus
- Coronary heart disease
- Preexisting hypertension.
Dosages of Common Medications Used to Prevent Urinary Calculi:
- Thiazide diuretics
- Hydrochlorothiazide 25 mg PO bid
- Chlorthalidone 25-50 mg PO daily
- Indapamide 2.5 mg PO daily
- Sodium cellulose phosphate 10-15 g/day divided with meals
- Orthophosphate 0.5 g PO tid
- Potassium citrate 20 mEq PO bid-tid
- Allopurinol 300 mg PO daily
- Magnesium gluconate 0.5-1.0 g tid
- Pyridoxine (B6) 100 mg PO daily
- D-Penicillamine 250 mg PO daily (titrated to effect)
- α-Mercaptopropionylglycine 100 mg PO bid (titrated to effect)
- Captopril 25 mg PO bid-tid
- Acetohydroxamic acid 250 mg PO bid-tid.
Potential Side Effects of Medications Used to Prevent Urinary Lithiasis:
| Medication | Side Effect |
|---|---|
| Thiazide diuretics, Hydrochlorothiazide | Potassium wasting, muscle cramps, hyperuricosuria |
| Chlorthalidone, Indapamide | Acidosis, hypocitraturia |
| Sodium cellulose phosphate | Gastrointestinal distress, hypomagnesemia, hyperoxaluria, parathyroid hormone stimulation, orthophosphate similar to sodium cellulosephosphate, soft tissue calcification. |
| Potassium citrate | Gastrointestinal upset, hyperkalemia |
| Allopurinol | Rash, myalgia |
| Magnesium gluconate, Pyridoxine (B6) | Diarrhea |
| D-Penicillamine | Nephrotic syndrome, dermatitis, pancytopenia |
| α-Mercaptopropionylglycine | Rash,asthenia,rheumatologic complaints, gastrointestinal distress, mental status changes |
| Captopril | Rash, cough, hypotension |
| Acetohydroxamic acid | Thromboembolic phenomena, tremor, headache, palpitations, edema, gastrointestinal distress, loss of taste, rash, alopecia, anemia, abdominal pain |
Medications Associated with Renal Calculus Formation:
Calculi Formed from Drug-- Indinavir
- Ephedrine
- Triamterene
- Magnesium trisilicate antacids (silicates)
- Sulfamethoxazole-trimethoprim
Calculi Provoked by Drug-- Carbonic anhydrase inhibitors
- Topirimate
- Furosemide
- Vitamin C (excess)
- Vitamin D (excess)
- Laxatives.